Amniocentesis & CVS
Amniocentesis and Chorionic Villus Sampling (CVS) are invasive diagnostic procedures that allow testing of fetal chromosomes. They are most commonly used to diagnose chromosomal abnormalities such as Down Syndrome but they can also be used to detect some inherited genetic disorders in high risk families.
Preparation
On the day of your appointment, you need to bring your referral and your blood group card, if you have one.
Why your bloodgroup is important
The majority of people have a Rhesus positive blood group and for women with a positive blood group undergoing prenatal testing, no special precautions are necessary. If you have a Rhesus negative blood group however, you will need an injection of anti-D after the procedure. This is given like a normal injection in your muscle. The reason why you need this injection is to stop you from making antibodies against Rhesus positive cells. Because most people are Rhesus positive, there is a good chance that your partner and therefore also your baby might be Rhesus positive. When we do a procedure, there is a risk that a few positive red blood cells of your baby may get into your circulation. Your body will recognise those positive cells as foreign and instruct your immune system to make antibodies to destroy them. Once your immune system has made these antibodies, they will be present for the rest of your life and can be a threat to this or subsequent pregnancies. They can cross the placenta and destroy the baby's positive red blood cells, causing anaemia and even death. When we give you an anti-D injection we basically give you anti-positive blood cell antibodies. These antibodies will clear up any positive red blood cells in your circulation before your immune system can be activated. Rhesus negative women need anti-D every single time there is a possibility that positive red blood cells go into their circulation: miscarriage, prenatal testing, bleeding in pregnancy, delivery of a Rhesus positive baby.
Anti-D is a blood product. It is made from blood of people who made antibodies at some stage in their lives. It is collected and processed in Australia by the red cross and is tested extensively for the different known infections. The advantages of having the anti-D far outweigh the possible small risk of having a blood product.
The procedure
Although most women find the procedure emotionally very stressful, the physical part is in general not very painful. The pain of an amniocentesis is comparable to that of a blood test. The pain of a CVS is mainly that of the local anaesthetic, which may sting when it is injected. This is probably comparable to a local anaesthetic at the dentist.
We usually recommend that a companion drives you home but most women are quite capable of driving themselves home if need be. You should organise to have some help at home so you can rest until the next day. There is however no need to go to bed.
You can experience some cramping of the uterus in the hours following the procedure. You can take panadol if this cramping is too uncomfortable.
If the cramping is more severe or if bleeding or fluid loss occurs, you need to contact either your referring doctor or the doctor who performed the procedure. Our doctors will give you a card with their contact details after the procedure. Don't hesitate to contact them if you are worried. They will organise an ultrasound to check the pregnancy as soon as possible.
Amniocentesis
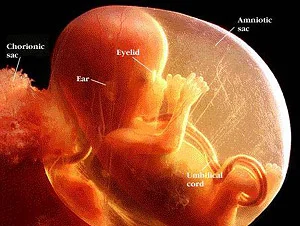
An Amniocentesis is an ultrasound guided procedure in which a small sample of the amniotic fluid is taken from the amniotic sac. The amniotic sac is the fluid-filled bag that surrounds the fetus.
Amniotic fluid contains cells from the fetus that have been shed from the skin, lungs and bladder.
An amniocentesis can be performed from 15 weeks gestation onwards. Before the amniocentesis, an ultrasound examination is performed:
- To check that the fetal heart beat is clearly seen
- To confirm the due date
- To assess if twins are present
- To localise the placenta and the fetus
- To check whether the fetus looks normal for the gestation
- To check the amount of fluid around the fetus
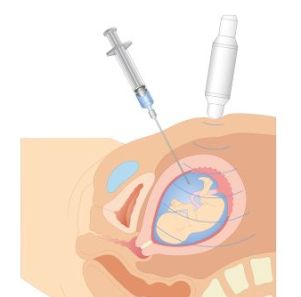
The skin is then cleaned with an antiseptic solution and a sterile bag is placed around the ultrasound probe. Under constant ultrasound guidance, a fine needle is inserted through the skin of the abdomen and the uterus, into the amniotic sac. It takes approximately 30 seconds to withdraw 15-20 millilitres of amniotic fluid. This fluid is quickly replaced by the fetus. A local anaesthetic is not required. The test is not very painful. Most women find the discomfort similar to that of a blood test.
After the amniocentesis, the doctor will recheck the fetal movements and heartbeat with ultrasound.
Although amniocentesis is a relatively safe procedure, it remains an invasive procedure and has therefore a risk of miscarriage associated with it. Miscarriage after amniocentesis occurs in about one in every 200-400 women tested. Miscarriage, if caused by the procedure, usually occurs within 2-3 weeks.
Temporary leaking of amniotic fluid after amniocentesis occurs occasionally.
A little bit of cramping is normal after the procedure but if severe cramping, bleeding or fluid loss occurs, the doctor who performed the procedure needs to be contacted and will organise an ultrasound to check the pregnancy.
Women with a Rhesus negative blood group are given an injection of anti-D after the procedures. This is to protect a woman with a Rhesus negative blood group from developing antibodies against a fetus whose blood group may be Rhesus positive.
Chorionic Villus Sampling (CVS)
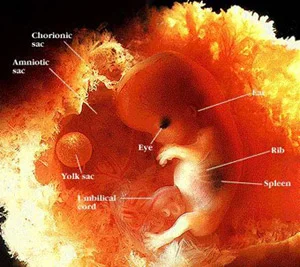
A CVS is an ultrasound guided procedure in which a small sample of chorionic villi are taken from the placenta. Chorionic villi are small thread-like projections that make up part of the early placenta. The cells of the chorionic villi almost always have the same chromosomes as the fetus.
A CVS is preferably performed between 11 and 14 weeks.
Before the CVS, an ultrasound examination is performed:
- To check that the fetal heart beat is clearly seen
- To confirm the due date
- To assess if twins are present
- To localise the placenta and see whether it is accessible for the test
- To check whether the fetus looks normal for the gestation
The skin is then cleaned with an antiseptic solution and a sterile bag is placed around the ultrasound probe. Under ultrasound guidance local anaesthetic is injected in the skin and the surface of the uterus. This is the most uncomfortable part of the test. Subsequently, a needle is inserted through the skin of the abdomen and the uterus, into the placenta. This needle remains in place for the duration of the test, usually 1-2 minutes. This is usually not painful. A second, finer needle is passed through the first needle and is used to draw up chorionic villi. Because the first needle remains in place and is used as a guide, a second or third aspiration can be done without any further trauma to the uterus.
After the CVS, the doctor will recheck the fetal movements and heartbeat with ultrasound
Occasionally, it happens that due to the position of the uterus or the placenta or due to early gestation, the placenta is not safely accessible. The doctor may then suggest another appointment in 1-2 weeks or an amniocentesis as an alternative test in those circumstances. In some centres in this situation, a vaginal CVS may be offered. In our practise transvaginal CVS is no longer performed because of the higher risk of miscarriage associated with this route.
Although a CVS is a relatively safe procedure, it remains an invasive procedure and has therefore a risk of miscarriage associated with it. Miscarriage after CVS occurs in about one in every 100-200 women tested. Miscarriage, if caused by the procedure, usually occurs within 2-3 weeks.
Occasionally transient bleeding occurs after CVS.
A little bit of cramping is normal after the procedure but if severe cramping, bleeding or fluid loss occurs, the doctor who performed the procedure needs to be contacted and will organise an ultrasound to check the pregnancy.
Women with a Rhesus negative blood group are given an injection of anti-D after the procedures. This is to protect a woman with a Rhesus negative blood group from developing antibodies against a fetus whose blood group may be Rhesus positive.
CVS or Amniocentesis?
The decision to have a CVS or amniocentesis is best made after discussion with your obstetrician and your partner. Both tests have their advantages and disadvantages. The main differences between CVS and amniocentesis are:
CVS
- Done between 11-14 weeks
- Earlier diagnosis
- Slightly more uncomfortable (minimal difference)
- Slightly higher risk of miscarriage associated with the test
Amniocentesis
- Done from 15 weeks onwards
- Later diagnosis
- Less uncomfortable (minimal difference)
- Slightly lower risk of miscarriage associated with the test
If you are uncertain as to whether you should have a prenatal test or which prenatal test you should have, feel free to make an appointment with one of our doctors for further counselling.
Laboratory tests
Banded karyotype
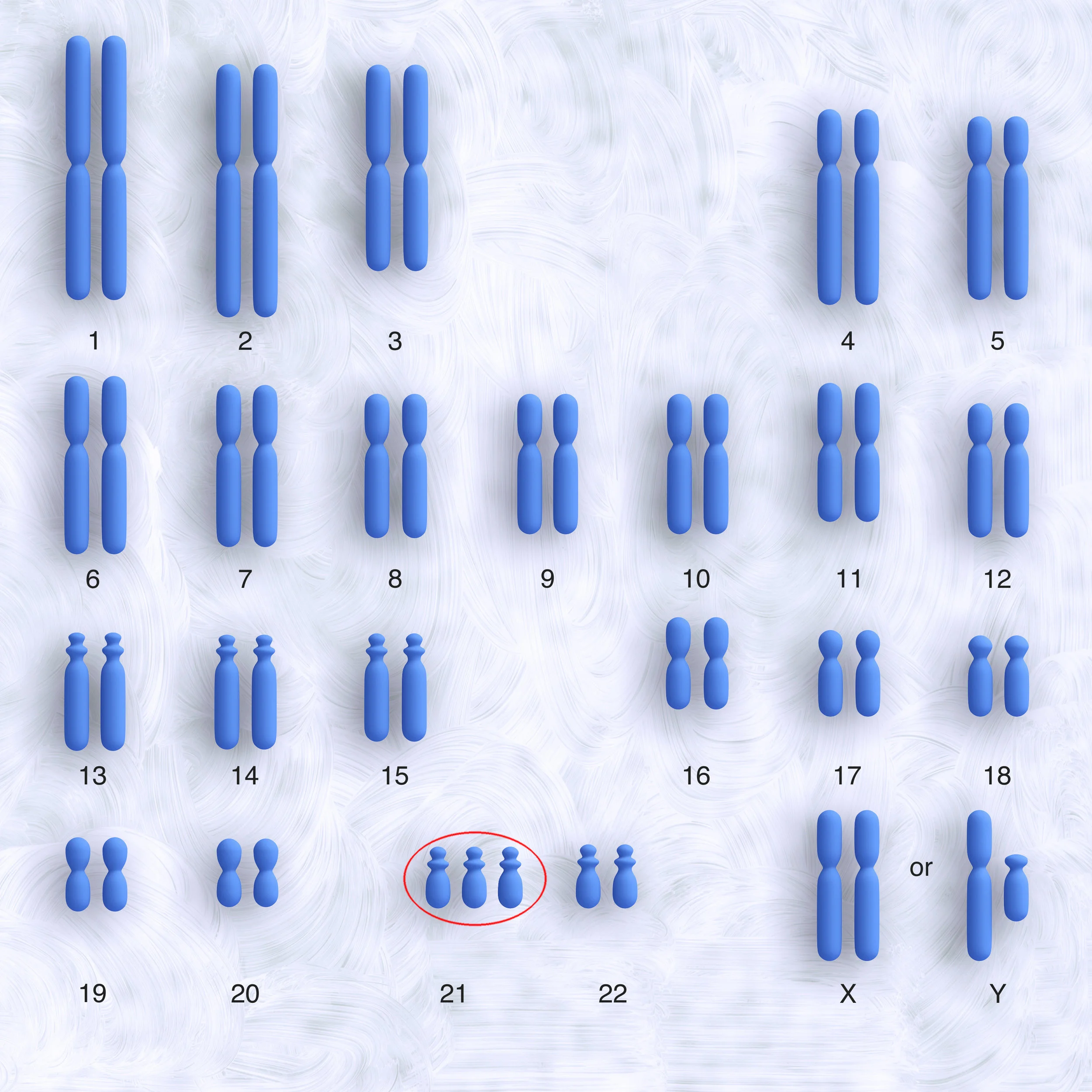
This test has been performed for many years. The cells collected by CVS or amniocentesis are sent to a cytogenetics laboratory. There the cells are cultured (stimulated to grow and divide) for 10-14 days. After enough cells are obtained, a banded karyotype can be performed. This means that the fetal chromosomes in the cultured cells are stained and subsequently photographed. The photographed chromosomes are then ordered by number, counted and checked for structural abnormalities. There should be 46 chromosomes, 23 pairs. A boy's karyotype is described as 46,XY and a girl's karyotype is described as 46,XX. In case of Down Syndrome, there is a third copy of chromosome 21.
It usually takes 2 weeks to get a result of the banded karyotype.
Micro array or molecular karyotype
Microarray, also called molecular karyotype, is a relatively new way of performing detailed testing of the genetic material contained in our chromosomes. Microarray is gradually replacing the banded karyotype.
Every cell in our body contains a full set of our genes on strands of DNA wrapped up in tiny bundles called chromosomes. These thousands of genes are collectively referred to as our genome. Whereas the older chromosome testing technique, banded karyotype, can only detect very large changes in our genome, microarray can detect much smaller variations, usually called 'copy number variants'.
This means that microarray is a very sensitive test which is generally helpful because it is able to detect more causes of developmental and other health problems. The increased sensitivity is occasionally problematic because some 'copy number variants' that are detected are not fully understood or have not been previously reported in the medical literature. In these instances it can be difficult for us to predict what the outcome will be, but testing of the parents and advice from a geneticist will be helpful in some cases.
If it is suspected that your unborn baby might have a chromosomal abnormality we will talk to you and your doctor about testing options, and help you decide whether a microarray or a banded karyotype would be the most appropriate test.
5-probe FISH (Fluorescent in Situ Hybridisation)
A 5-probe FISH can be done in addition to the banded karyotype or micro array.
A 5-probe FISH offers a rapid result, within 24-48 hours for particular chromosomes. It tests for the number of chromosomes 13, 18, 21, X and Y.
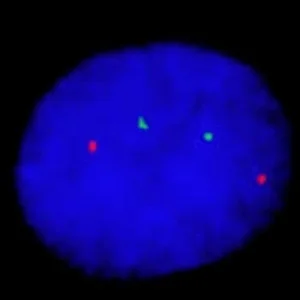
Fluorescent stains of different colours are mixed with fresh cells obtained by CVS or amniocentesis. These different coloured stains will bind with chromosome 13, 18, 21, X and Y. The cells are then studied under the fluorescent microscope. In a normal cell there should be 2 fluorescent dots of the colour representing chromosome 13, 2 dots representing chromosome 18, 2 dots representing chromosome 21 and 2 dots representing the X chromosome if the fetus is female and 1 dot for the X chromosome and 1 dot for the Y chromosome if the fetus is male.
In case of trisomy 21 or Down Syndrome, three dots representing chromosome 21 are seen, as in the picture below (the pink dots represent copies of chromosome 21).
There will be an extra charge by the laboratory for a 5-probe FISH.
The 5-probe FISH result will always be followed by a complete banded karyotype or micro array.